very day, new technologies emerge that are designed to make it easier for people to connect with the things they need, and healthcare is no exception. Today’s tech-savvy patients are using digital means to make appointments, check test results, remember to take medication, get answers to health-related questions, and more.
Healthcare facilities are also using updated technology to run offices and practices more smoothly, using artificial intelligence (AI) to ensure equipment remains up and running, and taking advantage of virtual training tools to provide staff with continuing education opportunities. And insurers are embracing new technologies to deliver a more positive customer experience.
“In the past, the chance of a machine such as an MRI going down because it needed maintenance was a fairly unpredictable thing,” explains Rob Reilly, vice president and general manager, US and Canada Services, GE Healthcare. “When it did happen, techs were dispatched to deal with the problem, but depending on where the equipment was, the fix could be hours or even days away.”
While technicians have had the ability to log in remotely on these machines to look at fault codes and diagnose issues for more than a decade, today’s AI algorithms monitor patterns in the fault detection modules to predict failures before they occur.
“We’ve been able to remotely connect to machines to provide remote triage for fifteen-plus years, but with the evolution of new technology, the smarts embedded in the newer machines have taken this to a whole new level,” says Reilly.
“This is a huge deal in Alaska, where things are logistically challenging,” he adds. “If we can anticipate a problem, we can manage where our teams need to be. And now that we have a local warehouse in Anchorage, we can even forward deploy the parts that are needed so that we can provide same-day service.”
According to Reilly, once a potential problem has been detected, the remote fix rate is approximately 35 percent to 45 percent, so teams don’t have to go to the hospital or clinic. “When we do need to send an engineer, about 80 percent of the time they already have a game plan and know exactly what needs to be done,” he says. “The days of seeing a technician working on a machine with parts spread out across the floor are largely gone.”
Using Insite as its core technology, GE’s AI suite includes OnWatch and Tube Watch. OnWatch monitors systems in real-time, looking at different parameters to determine potential problems.
“It’s sort of like ADT monitoring for your home,” says Reilly.
For example, because it’s important to keep MRIs super-cooled, AI technology monitors the magnets inside to make sure that the machines do not overheat. “During last year’s hurricanes in the southeastern United States, we were constantly monitoring and remotely adjusting MRIs to help these devices ride out power outages for twelve to eighteen hours without quenching and losing helium,” says Reilly.
OnWatch reduces unplanned downtime by approximately 35 percent by preventing unscheduled disruptions. “Even when we can’t repair the equipment remotely, it’s still 30 to 40 percent faster when we dispatch a technician because they already have a game plan,” says Reilly.
Tube Watch, an AI technology used in CT scanners, helps monitor tube life. “The tube inside a CT scanner generates radioactive beams, but it is a consumable, like a light bulb,” explains Reilly. “It will wear out after a certain number of scans, though this number can be unpredictable based on how many scans are done, how long they take, and how the machine is maintained.
“The CT scan is the first line of defense for trauma patients in the emergency room—if the tube goes, it’s typically an eight-hour job once you have a replacement tube,” he adds. “If an ER machine has to be down for eight hours, the hospital may need to go on divert.”
GE Healthcare
“With the AI digital twin running, we can accurately predict tube failures with about 80 percent accuracy within 72 hours of an event,” says Reilly. “This allows us to forward deploy parts so that they are available when needed. We can change a tube after-hours or on a Saturday when we can minimize disruption to patient schedules.
“Before we had the Anchorage warehouse and the ability to predict upcoming failures, a tube could go down at 9 a.m. on a Thursday and, in some cases, we wouldn’t be able to get it fixed until Monday,” he adds. “You’re talking days of downtime. And now we’re talking hours. It has had a dramatic impact.”
This capability even extends to facilities in Bush villages, where working equipment can mean the difference between life and death. “Many Alaska hospitals have this technology, including in Southcentral Alaska and in a number of Southeast villages, but the biggest benefit is in far north villages such as Barrow and Nome,” says Cody Pittman, GE’s service director for Alaska.
Through GE’s partnership with Norton Sound Health Corporation, it has installed a state-of-the-art MRI in Nome with this technology, which is one of GE’s most remote MRI installations in the world.
“Now that we have CT scanners with this technology in Barrow and Nome and an MRI in Nome, we are able to offer Lower 48 metro-level service delivery to Bush villages in Alaska,” says Pittman. “In the case of an emergency, it’s incredibly valuable to know that they have scanners with minimal downtime to prevent life-flighting a critical patient out of the village.
“Our customers bring patients in from smaller villages,” he adds. “Bringing this technology to Bush villages has resulted in lower wait times, and they no longer have to travel to Anchorage for outpatient scanning.”
In addition to possibly saving lives, the use of AI technology saves money. “Without Tube Watch, a facility is probably looking at a minimum of twelve hours of downtime,” says Reilly. “In Alaska, which has relatively lower patient volumes than in the Lower 48, that may mean about twelve to fourteen patients affected per day, meaning a loss of $5,000 to $10,000 in revenue.”
“In the past, using these high-tech machines required a very knowledgeable GE specialist who flew around the country teaching hospitals how to use it,” says Reilly. “But even if an expert was onsite for a week, after he or she left, there was a large decay curve of how much users could remember.”
Virtual technology not only provides the opportunity for users to revisit what they were taught but also to expand their knowledge. “Medical equipment is like your phone or computer at home—a lot of people may know the basics, but they are not harnessing 80 percent of the power it has,” he adds.
Because of lower patient volumes, hospital staff may not be as familiar with the equipment as they would be in busier areas.
“Healthcare facilities in rural areas don’t see the volume of cases—for example, head injuries—like they would in somewhere like New York, so hospital staff may not be as familiar with the different software and the way to properly position a patient,” says Reilly.
For this reason, some cases may need to be re-scanned, and using virtual training can lessen that likelihood. “It also enables more advanced techniques that can give physicians and radiologists better scans, allowing them to harness the horsepower of this advanced technology,” he adds.
Virtual training is used across GE’s entire portfolio of equipment, including CTs, MRIs, patient monitors, mammograms, and ultrasound equipment. “It will never replace hands-on, one-on-one training, but we’ve seen improvements at facilities using it to augment that training,” says Reilly, adding that this service is available for purchase when facilities buy new equipment and can also be included in long-term service agreements.
“On the device side, we’re doing a lot of research with academic institutions to come up with new ideas,” says Reilly. “For example, studies are now being done to use different AI techniques during MRI exams to extrapolate information from less intensive scanning.”
A typical MRI can take forty-five minutes, but with AI it’s possible to acquire a smaller dataset faster and arrive at the same results. “Using AI, an MRI might be able to use far less data than we would normally acquire and use deep learning from tens of thousands of images to build out full scans,” says Reilly. “Radiologists have been blown away by looking at AI-enhanced MRIs compared to full MRI exams; in many cases they can’t tell the difference. This would create a significant difference in patient throughput and patient comfort without sacrificing quality.”
This could also allow hospitals to handle much higher patient volume using fewer machines.
“The Alaska market is exciting because the employer population understands that the high cost of healthcare and remote access is creating barriers to care, and they want to get digital tools out to their employees to make it easier for them to find and access the care they need,” says Patti Brooke, director of innovation at Premera Test Kitchen. “As we run new digital pilots, we see a very high level of engagement.”
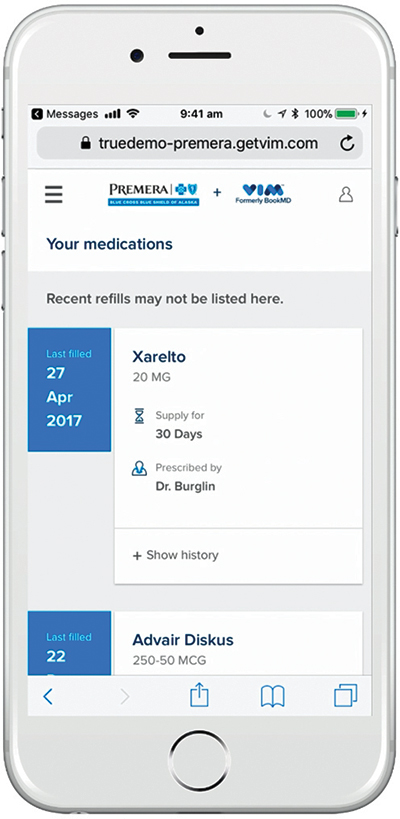
Premera Blue Cross Blue Shield of Alaska
In early June 2019, Premera launched a pilot program for MyCare Alaska, which allows users to find and connect with a physician in real-time to resolve their healthcare needs. Users can download the iOS or Android app, list their symptoms, and shortly thereafter text with a doctor to determine a course of care.
“MyCare Alaska gives Premera customers immediate access to physicians, which is especially important for those living in remote areas or who have challenges with physician availability,” says Brooke.
The pilot program is currently available to about 20,000 fully insured large group members, and the company is collecting feedback from members and providers for future iterations of the product. Both Premera Pulse and MyCare Alaska are SOCQ and HITRUST-certified to make sure that patients’ medical information is kept safe.
Premera Scout, which was launched in January 2018 on Premera’s Android app and the following July on Premera’s Facebook page via Messenger, is a virtual assistant that uses easy-to-understand, text-based chat conversations to help customers find information on claims, benefits, and other Premera services.
“The cool thing about it is that you don’t have to use insurance jargon to ask your questions,” she adds. “It uses a form of AI natural language processing that can understand users’ questions in their own words, even if services are described in a different way.”
Premera’s digital customer experience team continues to build capabilities to provide a chat service through its mobile apps, as well as to connect to users’ specific accounts for direct answers instead of links to places where answers can be found. The virtual assistant, which was designed in conjunction with Microsoft Healthcare NExT, has already won several awards, including the 2019 Microsoft for Healthcare Innovation Award.
“We’re still in the early stages of AI in healthcare, and we’re working with predictive analytics and new algorithms to apply it to data to better forecast the health needs of our members,” says Brooke. “The fact that we now have so much data gives us the opportunity to make navigating the healthcare system much easier and more efficient, increasing patient satisfaction and decreasing costs.” ![]()